Osteochondral Reconstruction: Surgical Treatment & Repair Training
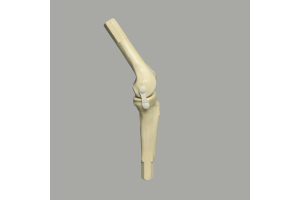
Osteochondral lesions are common among both the young and the old. These cartilage tears can be caused by multiple scenarios, including injury, trauma, and osteonecrosis, among others. Accurate anatomical models help train and sharpen residents' skills in osteochondral reconstruction procedures such as the osteoarticular transfer system (OATS). Let's take a closer look.
Osteochondral Reconstruction
When defects or trauma damage only a part of the knee, patients can opt for a procedure that reconstructs the affected part instead of replacing the entire cartilage and bone. Treatment procedures include rest and immobilization, microfracturing, autologous cartilage implantation, and osteoarticular transfer system (OATS).
- Non-surgical treatment - First-line treatment involves joint immobilization and rest. Nonsteroidal anti-inflammatory drugs (NSAIDs) may be used to stop further damage. Non-surgical treatment is particularly suitable for young patients and adolescents, as their growing bones have a higher chance of complete healing after rest.
- Microfracturing - Small lesions are treated by drilling tiny holes or microfractures in the bone to facilitate the entry of fibrous cartilage into the affected area.
- Autologous cartilage implantation - Surgeons can also fill in small holes by implanting cartilage cells harvested from the patient and grown separately in a petri dish.
- Osteoarticular transfer system - OATS is recommended for lesions typically larger than 10 mm on the articular surface of the knee bone. These larger, isolated lesions are filled with healthy cartilage and bone harvested from the non-weight-bearing portions of the knee bone. Healthy cartilage and bone can come from the patient (autograft) or a donor (allograft).
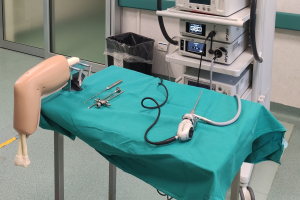
OATS has been traditionally practiced as an open procedure. However, advances in arthroscopic techniques and tools have allowed a less invasive approach to treating osteochondral lesions. Anatomical models help residents and medical professionals develop the highly precise arthroscopic skills necessary for a successful osteoarticular transfer system procedure.
Practicing Arthroscopic OATS Procedure With Anatomical Models
Models help residents and medical professionals build and develop skills in performing technically demanding arthroscopic techniques, such as visualization, harvesting, and graft placement. Below are some of the ways anatomical models raise the level of class instruction and discussion in OATS training:
|
Diagnostic Arthroscopy |
Models demonstrate the proper location of landmarks for the incision and introduction of arthroscopic instruments. Residents can use models to explore the anatomical structure of the knee in relation to diagnostic arthroscopic techniques, such as the resectioning of the fat pad, for proper visualization and cartilage harvesting. The manipulation of arthroscopes, shavers, and other instruments for debridement and removal of lesions can be practiced on anatomical models. Instructors can emphasize best practices such as fully visualizing and assessing the thickness of the lesion, avoiding general bleeding in the bone, and clearing remaining residues of articular cartilage from the subchondral bone. |
|
Graft Harvesting |
Models allow residents to practice the visualization and harvesting of graft material from the donor site. Foam models, suited to drilling and cutting, allow for the hands-on practice of graft sizing, drilling, malleting, cutting, and removal of the graft for transfer. Models also familiarize residents with arthroscopic instruments including OATS harvesters, sizers, probes, mallets, and others. Instructors can discuss best practices such as positioning the harvester assembly perpendicularly to the donor site, confirming alignment from multiple angles, and the proper backfilling of donor sites to avoid degeneration. |
|
Graft Transfer and Placement |
Residents can practice graft insertion into the recipient site using anatomical models. Preparation of the recipient site by drilling to the appropriate depth can be demonstrated. The use of harvesters, delivery tubes, and bone tamps can be repetitively practiced on models to ensure proper placement and fit. Instructors can use models to call attention to best practices such as flexing the knee to ensure perpendicular placement of the guide to the lesion, using a gentle but firm force to introduce the graft, and ensuring a well-contoured appearance with the graft flush with nearby cartilage. |
|
Discussion |
Bone models facilitate in-depth discussions of the procedure's advantages and disadvantages, including the ones below: Advantages
Disadvantages
|
In summary, anatomical models improve instruction in OATS training programs for the treatment of osteochondral lesions. Models familiarize residents with the knee’s anatomical structure in relation to the arthroscopic procedure and help residents visualize arthroscopic techniques and their advantages and disadvantages. Foam models, which are designed for cutting and drilling, also facilitate hands-on training with arthroscopic tools and instruments, even before residents enter an operating room. Lastly, anatomical models help residents and medical professionals develop the precision in procedural skills demanded by an arthroscopic approach to OATS.
Best-In-Class Anatomical Models
Sawbones designs and manufactures best-in-class anatomical models for residents, instructors, students, sales specialists, and more. We offer customized products, including models and custom displays, for residency program needs. Sawbones is a proud partner of several medical training institutions, including the Postural Restoration Institute® and Medical Sales College.
Sawbones offers the best-in-class anatomical models for practicing osteochondral reconstruction procedures such as OATS. For more information on our offerings or to talk about custom training models, contact us at 206-463-5551.